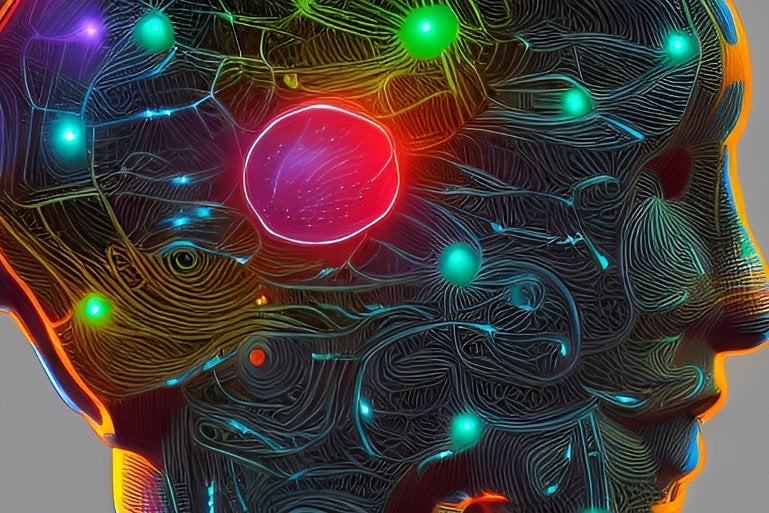
Summary: COVID-19 an infection prompts the identical inflammatory response within the mind as Parkinson’s illness, a brand new research experiences.
Source: University of Queensland
Research led by The University of Queensland has discovered COVID-19 prompts the identical inflammatory response within the mind as Parkinson’s illness.
The discovery recognized a possible future threat for neurodegenerative situations in individuals who’ve had COVID-19, but additionally a doable therapy.
The UQ staff was led by Professor Trent Woodruff and Dr. Eduardo Albornoz Balmaceda from UQ’s School of Biomedical Sciences, and virologists from the School of Chemistry and Molecular Biosciences.
“We studied the effect of the virus on the brain’s immune cells, ‘microglia’ which are the key cells involved in the progression of brain diseases like Parkinson’s and Alzheimer’s,” Professor Woodruff stated.
“Our team grew human microglia in the laboratory and infected the cells with SARS-CoV-2, the virus that causes COVID-19.
“We found the cells effectively became ‘angry,’ activating the same pathway that Parkinson’s and Alzheimer’s proteins can activate in disease, the inflammasomes.”
Dr. Albornoz Balmaceda stated triggering the inflammasome pathway sparked a “fire” within the mind, which begins a persistent and sustained means of killing off neurons.
“It’s kind of a silent killer, because you don’t see any outward symptoms for many years,” Dr. Albornoz Balmaceda stated.
“It may explain why some people who’ve had COVID-19 are more vulnerable to developing neurological symptoms similar to Parkinson’s disease.”
The researchers discovered the spike protein of the virus was sufficient to begin the method and was additional exacerbated when there have been already proteins within the mind linked to Parkinson’s.
“So if someone is already pre-disposed to Parkinson’s, having COVID-19 could be like pouring more fuel on that ‘fire’ in the brain,” Professor Woodruff stated.
“The same would apply for a predisposition for Alzheimer’s and other dementias that have been linked to inflammasomes.”
But the research additionally discovered a possible therapy.
The researchers administered a category of UQ-developed inhibitory medication that are at the moment in medical trials with Parkinson’s sufferers.
“We found it successfully blocked the inflammatory pathway activated by COVID-19, essentially putting out the fire,” Dr. Albornoz Balmaceda stated.
“The drug reduced inflammation in both COVID-19-infected mice and the microglia cells from humans, suggesting a possible treatment approach to prevent neurodegeneration in the future.”
Professor Woodruff stated whereas the similarity between how COVID-19 and dementia ailments have an effect on the mind was regarding, it additionally meant a doable therapy was already in existence.
“Further research is needed, but this is potentially a new approach to treating a virus that could otherwise have untold long-term health ramifications.”
The analysis was co-led by Dr. Alberto Amarilla Ortiz and Associate Professor Daniel Watterson and concerned 33 co-authors throughout UQ and internationally.
About this COVID-19 and neuroinflammation analysis information
Author: Press Office
Source: University of Queensland
Contact: Press Office – University of Queensland
Image: The picture is within the public area
Original Research: Open entry.
“SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein” by Eduardo A. Albornoz et al. Molecular Psychiatry
Abstract
SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia by means of spike protein
Coronavirus disease-2019 (COVID-19) is primarily a respiratory illness, nevertheless, an rising variety of experiences point out that SARS-CoV-2 an infection also can trigger extreme neurological manifestations, together with precipitating circumstances of possible Parkinson’s illness.
As microglial NLRP3 inflammasome activation is a serious driver of neurodegeneration, right here we interrogated whether or not SARS-CoV-2 can promote microglial NLRP3 inflammasome activation.
Using SARS-CoV-2 an infection of transgenic mice expressing human angiotensin-converting enzyme 2 (hACE2) as a COVID-19 pre-clinical mannequin, we established the presence of virus within the mind along with microglial activation and NLRP3 inflammasome upregulation compared to uninfected mice.
Next, utilising a mannequin of human monocyte-derived microglia, we recognized that SARS-CoV-2 isolates can bind and enter human microglia within the absence of viral replication.
This interplay of virus and microglia instantly induced sturdy inflammasome activation, even within the absence of one other priming sign. Mechanistically, we demonstrated that purified SARS-CoV-2 spike glycoprotein activated the NLRP3 inflammasome in LPS-primed microglia, in a ACE2-dependent method.
Spike protein additionally might prime the inflammasome in microglia by means of NF-κB signalling, permitting for activation by means of both ATP, nigericin or α-synuclein. Notably, SARS-CoV-2 and spike protein-mediated microglial inflammasome activation was considerably enhanced within the presence of α-synuclein fibrils and was solely ablated by NLRP3-inhibition.
Finally, we reveal SARS-CoV-2 contaminated hACE2 mice handled orally post-infection with the NLRP3 inhibitory drug MCC950, have considerably diminished microglial inflammasome activation, and elevated survival as compared with untreated SARS-CoV-2 contaminated mice.
These outcomes help a doable mechanism of microglial innate immune activation by SARS-CoV-2, which might clarify the elevated vulnerability to growing neurological signs akin to Parkinson’s illness in COVID-19 contaminated people, and a possible therapeutic avenue for intervention.














Discussion about this post